Like their parents, Latinx youth are suffering disproportionately from COVID
 October 29, 2020
Category: Featured, Long, Purpose
October 29, 2020
Category: Featured, Long, Purpose
As we enter the virus’ third wave, COVID -19 has ravaged the country. It is estimated that deaths from COVID-19 will reach 400,000 by the end of the year, but children have — by and large — been spared its harshest symptoms. Most youth have mild cases that don’t require hospitalization.
Yet a recent Center for Disease Control and Prevention (CDC) report shows that Latinx children were more likely to be hospitalized, and that they suffered the highest death rate from COVID-19 than children from any other races or ethnicities.
Of almost five million U.S. positive COVID infection cases reported, about 265,000 where reported in youth younger than 17 years old. Of those cases, there have been only 121 deaths reported. Yet, the pediatric burden of COVID-19 is not shared equally.
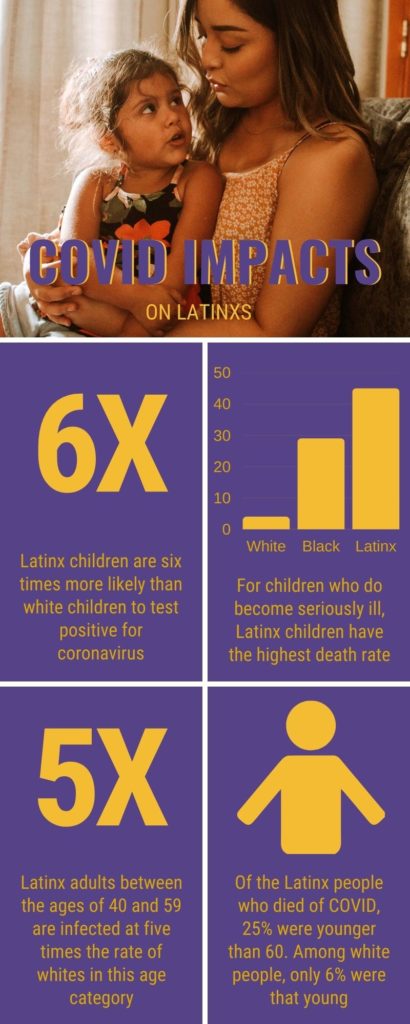
Latinx children are six times more likely than white children to test positive for coronavirus. This makes them the pediatric group most at risk for contracting the virus. And for the children who do become fatally ill, Latinx children have suffered the highest death rate —45% compared to 29% for Black and 4% for white children.
Like their parents, Latinx youth are suffering disproportionately from COVID.
Latinx adults, too, are more likely to lack access to testing; to get COVID-19; to suffer from more severe cases; and to die, than the general public. Latinx adults between the ages of 40 and 59 are infected at five times the rate of whites in this age category, CDC data showed. Of the Latinx people who died of COVID, 25% were younger than 60. Among white people, only 6% were that young.
“The disparities that were initially recognized among adults with COVID are the exact same disparities we see with children of color,” said Dr. Susan E. Coffin, the attending physician for the Division of Infectious Diseases at Children’s Hospital of Philadelphia.
She added, “Black and brown children are more likely to get infected, require hospitalization if infected, and even require intensive care unit care.”
For the most seriously ill, those whose COVID infection leads to the severe complication called multisystem inflammatory syndrome in children (MIS-C), Latinx children still have the highest rate of occurrence.
“I would guess (although cannot easily find data to confirm this) that higher complication rates in Hispanic and non-Hispanic Black children reflect higher COVID-19 positivity rates in Hispanic and non-Hispanic Black children in general,” said Dr. Daria Chacón, associate medical director for Health Information Management, and attending physician in Internal Medicine and Pediatrics for Esperanza Health Center.
“To me, it seems likely that closer proximity in our housing and the large number of intergenerational households play a role in the higher positivity rates we see in our practice, compared with the city as a whole,” she said.
Latinxs are 14.1 percent of the city’s population but it is also a community that has some of the city’s poorest health outcomes. As we are entering the third wave of the pandemic, these issues will continue to cause disparate rates of illness in minority communities.
Some of those issues:
- Underlying health conditions. One out of four children who died were previously healthy with no reported underlying medical condition, but 75% had at least one underlying medical condition, including asthma.“Because our patients also tend to have a disproportionate burden of asthma and other chronic illness, they tend to become sicker with COVID-19 than the average patient,” said Dr. Chacón. “These are factors we can’t change quickly.”
- Essential workers. Many Latinx parents work in service positions and are considered essential frontline workers. “Adults of color are more likely to be exposed to COVID due to their work in essential roles [and] increased reliance on public transportation,” Dr. Coffin explained. “And families of color may have more challenges getting tested, which can delay recognition of the need to quarantine or isolate.”
- Lack of health insurance. Less than half of Latinxs have access to private health care, the lowest of any demographic group, according to the report The Impact of COVID-19 on Latinos in the U.S. from the Labor Council for Latin American Advancement.
- Unable to isolate. Transmission of the coronavirus within the household can be very high but multigenerational households are very common among minority populations, resulting in an increased risk for older individuals living with grandchildren. Isolating a sick family member is the best practice but for large families in small spaces, it is practically impossible. “Our patients tend to be quite careful about wearing masks and even gloves when they leave their homes,” said Dr. Chacón, “but may forget that close personal contact with a coworker or family is far riskier than casual contact with supermarket shoppers.”
Make the Road Pennsylvania, the largest Latinx organization in the state of Pennsylvania, released a new report this week, Unemployed, Unhoused, and Unhelped: COVID-19’s Devastating Toll on Pennsylvania’s Latinx Communities detailing the staggering economic devastation for Latinx Pennsylvanians and the fact that crucial government benefits are not reaching those who need them most.
The burden of the pandemic is also taking its mental health toll. As of July 2020, the Latinx population was eight percentage points more likely than the US white population to report symptoms of depression or anxiety.
Protecting children
“At this point, it appears that children are more likely to get COVID-19 from others in their home or from get-togethers outside of school,” Dr. Coffin said. Without a vaccine, prevention is still the best weapon in the medical arsenal of fighting this virus.
“While children are less likely get severely ill than are adults, their illnesses are still very important to prevent. Children’s infections can spread easily, particularly within a household, putting their older and more vulnerable household members at risk,” added Dr. Coffin.
For her part, Dr. Chacón said, “I would urge all parents to cautiously assess optional activities, avoiding those that involve close personal contact, unmasking, or high-risk activities such as singing.”
Hand hygiene, social distancing and mask wearing are still the critical lessons to teach children.
“There’s also some good news; very young children (younger than approximately age 2) probably do not transmit COVID-19 very effectively, and recent data shows that children are probably not the major drivers of transmission,” Dr. Chacón said.
For children over two years old, the CDC recommends wearing a mask.
“I think that critical step is to make sure your children know how important wearing their mask is,” Dr. Coffin advised.
Project
COVID-19 coverageTrending News